A Glimpse at FDA’s Micro Regulations
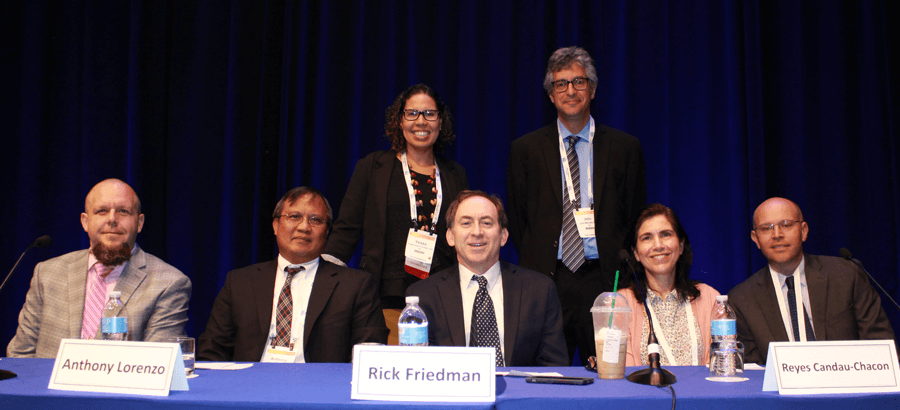
The 2019 PDA Global Conference on Pharmaceutical Microbiology closed with an engaging “Ask the Regulators” panel. Yeissa Chabrier-Rosello, PhD, Microbiologist, CDER, U.S. FDA, and John W. Metcalfe, PhD, Master Microbiology Reviewer, CDER, FDA, moderated the panel of FDA experts, which featured John T. Arigo, PhD, Branch Chief, CDER, Reyes Candau-Chacon, PhD, Quality Assessment Lead, CDER, Rick L. Friedman, Deputy Director, OMQ, CDER, Anthony F. Lorenzo, Lead Consumer Safety Officer, CBER, and J. Kevin Rice, PhD, Review Chemist, CVM.
Throughout the conference, attendees could submit questions on cards to be read during the session. This is a popular session of the microbiology conference, and, if you missed it, consider attending the 15th Annual Global Conference on Pharmaceutical Microbiology, Oct. 19–21, in Washington, D.C.
The following is a lightly edited transcript of the session with the identities of the questioners hidden. The panelists were given an opportunity to review their answers.
[Editor’s Note: This is an abridged summary of FDA responses during a panel dialogue at a conference. The responses below are an informal synopsis of the panel’s opinions and should not be construed to represent FDA’s views or policies.]
Question: Are there any expectations for freeze-dried products to be terminally sterilized after lyophilization?
John Arigo: The answer to that is, no. There is no expectation to be terminally sterilized after lyophilization.
Question: Has FDA received any successful methods for validating low endotoxin recovery (LER)?
Reyes Candau-Chacon: Yes. We received one application where the drug product could not be detected using the standard LAL-BET method. The applicant committed to developing a method capable of detecting endotoxin from the drug product. It took them two years to develop and validate the new method. T here are currently commercial endotoxin kits to help solve LER. The applicant used one of those kits as a starting point, eventually developing their own.
Our current expectation is to verify whether you can recover endotoxin spiked in the undiluted drug product. If the drug product has LER, we ask the applicant to develop a new method capable of detecting endotoxin from the drug product. We also ask applicants to inject endotoxin-spiked drug product into rabbits (a one-time study) to make sure the endotoxin that cannot be detected with the standard method does not result in a fever in the rabbits.
If the rabbit develops a fever, we ask the applicant to implement, as an interim test, the rabbit pyrogen test until the new method is developed, because a pyrogen test is a regulatory requirement. We also ask them to implement stronger microbial control of the process as an additional risk mitigation strategy.
Rick Friedman: We actually had a recall in the last two years that relates to what Reyes [Candau-Chacon] was speaking of. The endotoxin test passed for all the lots, but pyrogenic reactions occurred in patients. In response to these adverse events, the firm investigated by testing products using the rabbit pyrogen test and the product failed the pyrogen test. T he company is still working on the issues, but they have found that there were steps upstream in which pyrogen load and removal needed to addressed. It appears the fermentation process caused the high load. I believe this was a gram-positive fermentation-based (Streptomyces) product. Purification steps were insufficient, and some redesign was necessary to improve pyrogen removal efficacy.
Candau-Chacon: I have one thing to add to that. Even if we ask the applicant to conduct the rabbit pyrogen test, we make sure that it is an interim test. The rabbit pyrogen test is very insensitive. It should be used only as the last resort.
Question: What kind of personnel monitoring do you expect to see in a “low-bioburden facility” in a Grade B room?
Friedman: That is hard to answer. What this omits is the actual intended use of the product. Does this “low-bioburden facility” produce a sterile drug or an in-process intermediate that precedes sterilization? Or is this a nonsterile product with low microbial limits for bioburden? And what is going on in the room? The nature of the facility, including the operation of the room, as well as the dosage form and intended use of the product are critical considerations. All these things are at the core of making a risk assessment and determining what kind of personnel monitoring and guidelines may apply to that room.
This is very hypothetical, but in principle, it is normally a cascading processing situation that culminates in a Grade B (ISO 7 operational) room. The gowning would be appropriate to the ISO level. What needs to be proven, of course, is that this really is a low-bioburden facility by showing it is well designed and controlled. If those two things are not true, we all know the low-bioburden status can change overnight.
So, the concept of a low bioburden facility with appropriately stringent personnel controls is a good one. The reason you want to do environmental monitoring in the first place is to have a baseline on an ongoing to basis to show that you are in a state of environmental control.
Because we often discuss personnel and overall environmental control in the abstract, I think one example of lost environmental control at a sterile facility is useful to mention. We have all heard about the NECC [New England Compounding Center] findings. The data at that firm clearly showed that they had lost environmental control. They began to have signals early on that they should have acted on, and they ultimately lost control of it in a big way. Part of the problem was they performed personnel and environmental monitoring too infrequently. Earlier that year, products began to be made with drifting state of control. By about May, however, they were clearly making drugs that had clear links to clusters of infection reports showing the products were killing people.
In nearly all cases, infections due to contaminated medicines are typically detected by the healthcare system only after substantial time elapses, if at all. In the case of NECC, by that point, numerous patients were tragically harmed. T his obviously illustrates why systems to ensure an ongoing state of environmental control are so important to prevent the potential for product contamination in the first place.
Question: If implementing a rapid method for product sterility, what is the best way to submit a post-approval change? Would you recommend a comparability protocol first or a Type C?
Anthony Lorenzo: From a CBER perspective, I am not really clear what product this is because that would make a pretty dramatic change when implementing a rapid micro method. So, I would recommend at least requesting a Type C f irst to alert the Agency about what the change is and to get the right personnel together for this possible change. Again, we deal with a lot of different types of products, and this could be a very good method in some cases. A comparability protocol would be a good start, if applying this method to several products. Because we would require data to be submitted, I do not think we would accept a CBE-0. Only a CBE-30 would be accepted so that we can review the impact to product before release for commercial use.
Question: For facilities that manufacture both human and animal drug products, what process is used to review 483 observations from an inspection?
J. Kevin Rice: The answer to that is, what type of inspection was carried out?’
Question: For joint CDER/CVM inspections, what are the responses for 483s?
Rice: Again, it depends on the type of inspection. For PAI surveillance inspections, whichever Center requested the PAI, will almost certainly review the firm’s responses. If it were a general surveillance inspection, as our process currently stands, that would go to CDER for the review. Now, that does not mean that there cannot be collaboration between the Centers. If there are responses or observations specific to animal drugs being manufactured in that facility, we would certainly work with CDER and the investigators to make sure that those responses are sufficient.
Question: If changing from one USP <85> approved method to a second USP <85> approved method, is it necessary to use a CBE for post-approval changes, or is noting it in an annual report enough, if it is a low-risk change?
Arigo: For a change like that, I would check the post-approval changes guidance but, to me, that is a CBE change that we would want to review.
Question: Why is there a trend to force applicants to reduce the release specification information for compendial endotoxin tests?
Candau-Chacon: Sometimes the endotoxin specification is in EU/mg for liquid products and, when we convert it to EU/mL, we find that the specification is unacceptably high. I remember one recent application with a proposed endotoxin specification of 600 EU/mL. I do not think that a drug product with 600 EU/mL of endotoxin is under microbial control. In that case, we asked the applicant to lower that to levels consistent with good microbial control. We also want the applicant to include the endotoxin contribution from the infusion solution in the specifications.
Arigo: As long as the math works out where you are in the range of five, it is going to be fine.
Question: When it comes to environmental monitoring of personnel, should sampling be at random periodic intervals during the process, and should it include sampling of cleaning personnel?
Lorenzo: First of all, I am not sure at what stage this is referencing. In more critical areas, such as fill/finish, monitoring is fairly critical for personnel. The thing to consider in personnel monitoring is, what kind of information are you going to gather from it? Are you going to evaluate impact if there is a positive, or if there is product contamination from your personnel? That is critical information you need to know.
With random periodic intervals, I am not sure if that is beneficial. It is better to understand when sampling is performed, such as after personnel enter the critical zone, and you can determine if the impact from an intervention is captured. Regarding sampling of cleaning personnel, in manual cleaning, there is a similar expectation to randomly evaluate the cleaning effectiveness as it is being performed.
Friedman: I have just one additional comment on random personnel sampling. T here is the possibility of gaming the system. In fact, we included a statement in the aseptic guidance about sampling bias because it has been cited in inspections many times. More specifically, there were 483 observations where we would see in practice—even in front of an FDA inspector—that a company would sample aseptic processing operator gloves only after they fully sanitized them with isopropyl alcohol (IPA).That defeats the purpose of the sample, unless you are doing a study of how effective IPA is.
So, I think it is good practice to add some periodic random checks when aseptic personnel are exiting. This would augment the baseline program and provide further confidence in microbial control. QA or QC departments often add some sort of random check every month just to make sure there is no sampling bias in routine monitoring. The findings may indicate the need for even more frequent random sampling by, quality assurance as well as increased oversight of routine personnel/ environmental monitoring activities.
Question: For a generic animal drug packaged in a multidose container, does the inuse statement for the higher-level drug apply to the generic drug if the vial is the same size?
Rice: We certainly look at in-use statements on animal drugs a bit different from human drugs. We have multiple patient sizes and body weights compared to humans. We also have drug products that can be packaged anywhere from single-use vials or ampoules to 1L vials for production animal drugs. We actually have a draft guidance for industry out now that talks about how to design and carry out inuse stability studies for new animal drugs. It is CVM specific. To this question, in particular, “Does the in-use statement have to match the reference listed drug,” the answer is emphatically, “no.” CVM considers the in-use statements totally data-driven for a drug product. The way we have inuse stability studies designed and laid out in the draft guidance speaks to the ability of container closure systems to maintain a safe and effective drug over than in-use period. That in-use statement is completely data-driven. The in-use statements for the generic will be based on the in-use study that is carried out for that drug product and container/closure system.
Question: When reviewing an NDA for a new small-molecule post-approval stability program, is FDA still accepting sterility testing at annual intervals?
Arigo: Yes, you can do a sterility test at regular intervals. There is no requirement for container closure integrity testing over stability.
Question: Is it okay to do container closure integrity instead of sterility during stability?
Candau-Chacon: Yes, it is. If you include the container closure integrity testing in your stability program, you do not have to test for sterility during stability, however, you still need to test for sterility at release.
Question: What are the expectations for endotoxin testing in INDs?
Candau-Chacon: For INDs, we ask for sterility and endotoxin at release because they are linked to safety. We do not require LER studies at the IND stage.
Question: What is FDA’s current thinking for storage times and growth promotion studies in the final drug product? Should this be included in an IND? It is required in a BLA.
Candau-Chacon: Sometimes lyophilized products are stored before use. If those drug product solutions are growthpromoting, microorganisms may enter during product manipulations and grow out of control. In BLAs, we ask the applicant to conduct growth promotion studies if they intend to store the solution longer than four hours. We do not ask for hold studies in INDs, unless the sponsor has information that suggests that the drug product solution is growthpromoting.
Question: What would be a good environmental control strategy for continuous manufacturing processes?
Friedman: I would want to know more about your product. Continuous manufacturing comes in all shapes and sizes. It covers different products, from injectables to tablets, from the highest theoretical risk to the lowest. Again, I would need more information. An environmental control strategy for continuous manufacturing likely means that you are going to want real-time data, and there is some good equipment out there that could augment your process knowledge in real-time to give you rapid data on environmental or in-process bioburden. I have seen such methods coupled with routine sampling using traditional methods to ensure microbial identification. A balanced overall program would support batch release evaluation by establishing the appropriate combination of controls to be performed.
When it comes to biotech, or any kind of process where you are worried about microbiological risk—which is many of them—it is really important to build quality into the process. Early identification of adverse process signals can be an integral part of the overall design. There are many opportunities to better leverage technology to improve detectability. Detectability of contamination using f inal product testing alone is limited, although it does still reveal many sterility failures each year. The sterility test is really crucial as the last in a series of controls to determine whether the product is suitable for the market. But some sterility problems could be missed, and advanced environmental monitoring technology, if used properly, could help provide data that can help prevent exposure of patients to a product that lacks sterility assurance.
For nonsterile products, there are a lot of other things to consider. There is a really good bioburden chapter in USP. It includes about 20 variables that should be looked at in terms of designing for quality and ongoing assurance of in-process bioburden control.
My last point is about liquid and semisolid products. This is a big topic on our guidance committee for nonsterile dosage forms. There have been real problems, particularly on the sanitary systems side, due to lack of circulation, ambient temperatures, choices of materials of construction, etc. I recommend that everybody with liquid and semisolid products ensure they have a good team of engineers and microbiologists with manufacturing knowledge who can contribute a really good understanding of sanitary design.
Question: Regarding cell and gene products, what are the most commonly seen issues?
Lorenzo: Cell and gene products are relatively new to the Agency in terms of the technology and processes and understanding the manufacturing process. There is a lot of exchange going on between the Agency and the sponsors through the formal meetings and through the IND process. I think the most important thing for the Agency to learn is probably the unique aspects of these products in order to formulate reasonable regulatory policies. In terms of the facility and the manufacturing process, some of the issues we see coming up are contamination control issues with the facilities. A lot of cell and gene therapies are rapidly moving from a clinical stage that features very manual operations. We see this has a lot of impact on the commercial operations when they do the scale-out.
One of the things we look at when you are claiming production scale is, can you demonstrate it? It is very difficult for us to license a single-patient dose scale-out to a hundred patient doses. We often see the sponsors do not have a lot of the expertise to do the scale-out, and they do not have the time to practice for the scale-out. T here is a lot of impact. For example, it is not just sampling one batch in bigger volumes than we saw in scale-up operations. T he challenge for the QC department in a scale out is harder since they to get to perform hundreds of batches in a product that has one batch for one patient.
I recommend sponsors] come into the Agency and discuss their plans. There is a big push to get to market and being able to produce in the quantities you need.
Question: Biologics for animals are regulated by the U.S. Department of Agriculture. Do you see this moving to CBER in the future?
Rice: I think it is important to make a distinction here. Certainly, animal vaccines are regulated by the USDA, but cell-based products, stem cell products, for example, are not regulated by USDA, they are regulated by CVM. I think that is important to note. I do not know of any plans to transfer these cell-based products to CBER.
Question: For container closure integrity testing, what is the FDA’s position on studies that do not use vacuum pressure but, instead, only subject test files to one or the other?
Arigo: I think, in general, we want to see both pressure and vacuum for the container closure integrity test.
Question: Are you seeing facilities using nondistinct water purification, such as by osmosis at upstream stages?
Candau-Chacon: Yes, we have seen f irms using highly purified water by reverse osmosis along with firms that use purified water for the upstream part of the manufacturing process. Firms not using WFI need to demonstrate that the water generation system is able to reduce endotoxins and bioburden. Water sanitization and storage at high temperature will help maintain microbial control.
Question: USP <60> Microbiological Examination of Non-Sterile Products Tests for Burkholderia Cepacia Complex will become effective Dec. 1. What about products already on the market?
We are stressing risk assessments on objectionable organisms including, but not limited to, B. cepacia. This is especially important for products that may be used in susceptible patient populations—neonates and babies, pregnant women, immunosuppressed transplant patients, and so on. B. cepacia is not going away.
Also, sometimes preventing objectionable contamination is not enough. Our medical officers addressed medical risks when there were contaminated antiseptic topical swab recalls several years ago. T hey recommended that hospital administrators buy sterile wipes if the wipes are used presurgically, or in other, similarly vulnerable, clinical settings.
John Metcalfe: From my perspective, I am very happy to see the USP chapter going in. For applicants that are submitting applications for nonsterile aqueous products, you can expect that, when the application comes in, if you do not have B. cepacia testing in your release specification, our reviewers will be sending you a note to put that in. I have not heard anything or spoken to anyone at CDER who has said we are going to have you go back and put that information into older approved applications. We would hope, as Rick [Friedman] pointed out, that this is something you are already doing under basic GMPs but, as far as I know, at this point, there will be no regulatory requirement to update your application for existing approved products.
Friedman: GMPs provide the basic standard that products must be tested for microbiological contamination that is objectionable in view of their intended use. As our posted communications have noted, B. cepecia testing would be required as a batch-release test depending on the product and its intended use. And any water system, of course, has to be routinely tested for total counts and appropriately monitored for objectionable microbes and in many cases, that monitoring program should include B. cepacia. Another thing we are looking at is: Are you doing the right test for B. cepacia? USP <60> should help firms establish the right testing approach.
Metcalfe: I am going to mention one other thing—and I am not going to belabor this point—but there were people who approached me at this meeting and asked about a tablet product that was recalled from the market due to contamination with Pseudomonas and Burkholderia. T he question that was asked of me was, “When this USP <60> goes in, will there be an FDA expectation that B. cepacia testing is performed on the water system for nonsterile drugs?” The comment was made to that, there is a line in the chapter that says the tests could be applied to testing water systems. I am not sure if that was from an older version but I went back last night and looked in the latest draft of the chapter that is going to be coming out, and I did not see anything in reference to water systems. Certainly, FDA’s position would be that we hope you are testing your water systems for the organism. But the publication of USP <60> alone does not create a requirement to test pharmaceutical water. FDA’s GMP requirements and the intended uses of your products determine that.
Question: What considerations do you recommend for a filling machine used for a variety of products?
Lorenzo: There are expectations for aseptic filling addressed in various guidance documents. When you start dealing with multiple varieties of products, it depends. On the CBER side, we see multiple types of virus vaccines being filled. This poses cross-contamination issues if you do not have proper line clearance and robust cleaning procedures. There is also a need to evaluate other products when you do not own the filling line. New product on a line needs to be reported to all the sponsors because of its potential to affect other products. Specifically, if you are a contract manufacturer, you are going to have to let your clients know what is going to be exposed in that facility. A sponsor would have to evaluate that impact and report it to the Agency.
The most critical thing to consider is the impact to the sterility of products. It is not unusual for filling lines to fill a variety of products and vial types. You should do a media fill simulation of the vials and vial types but you do not have to do all of them. If you can provide the rationale and the justification, it will probably be easier to apply a bracketing approach. T here are also considerations for cleaning, making sure that materials that are touching multiple products are not going to pass residue from other products.
Question: The 2004 FDA guidance only requires 0.5 or greater micron particles for monitoring cleanroom classification. For GMP, Annex 1 also requires 5.0 micron. My question is, Does FDA have any plans to start requiring the 5.0 micron particle as a metric?
Friedman: In the early part of the 21st century, we met with our European colleagues who were working on an earlier version of Annex 1. Our goal, as we wrote the aseptic guidance at that time, was to endeavor to make the guidances equivalent. We accomplished that. But the FDA guidance and Annex 1 do not have to be identical, and our guidance is silent on a few topics, including 5.0 micron. From our point of view, it was difficult to determine an exact magic number that is objectionable, but that does not mean you should ignore a significant issue with 5.0 micron particles as a matter of control. So, what we can say is that it is important to look at 5.0 microns in certain cases. If the results are abnormal in an ISO 5 area, you should look into why it is occurring.
If you use regulatory guidance as the f inite cookbook to tell you what to do, this feeds a misconception that rote or checkbox compliance is all you need to do to make sure each batch of products are manufactured to be safe and effective. There is no comprehensive checklist that this is “all the things FDA told me to do, and I now can sleep soundly at night because I checked those boxes.” You have to follow good science and monitor the signals in your operations, and do all the things that you have to do.
Question: Can I use a rapid microbial test method for my water system and water for injection in parallel with traditional plate count tests, even if the rapid test has not been validated?
Friedman: With PAT [process analytical technology], the industry was worried about being innovative with more sensitive methods and thought the results of potentially more sensitive tests would trigger a disproportionate response during inspections. That is one of the reasons why CDER and ORA staff were trained in this area, and we also have processes within ORA and CDER involving preapprovals and compliance evaluations.
The bottom line is, we did address it in the PAT guidance toward the end of the document. There is close to a quasi-safe harbor for you to do side-by-side testing during the research phase. The exception, of course, is in the highly unlikely event that a legitimately serious hazard was revealed by the testing; it would then be incumbent on any responsible firm to take action and investigate, if appropriate. The PAT approach was intended to encourage interest in a technology that may be beneficial. We encourage innovative methods, including rapid methods, that are suitable for their intended use.
Lorenzo: I want to say from a CBER perspective, particularly around cell and gene therapy products, we encourage it because it reduces the risk to the patient, who is receiving the product almost immediately, and there is no way for traditional testing evaluate it. The patient cannot wait that long.
Work with the Agency, discuss your plans and proposals with us. We just need to know that what you are choosing is comparable, if not better.


