In-process Microbial Control During Aseptic Processing (High-Risk)
Last year, 37 microbial contamination recalls were listed on the U.S. Food and Drug Administration (FDA) Drug Recalls website. Since the Microbial Control of Raw Materials Used in Pharmaceuticals article was published (1), five recalls of sterile drug products due to microbial contamination have been added, and three people have died due to eye infections caused by contaminated products (2). Obviously, there are still practices being employed by some drug manufacturers that pose the risk of contamination for sterile drug products. This article will address best practices that should be employed to further reduce the risk of microbial contamination of sterile drug products and bacterial infections in patients.
Looking at current practices that are used in the manufacture of sterile injectable drug products, there are three general risk classes based on the presence of personnel in proximity to open containers and routes of exposure to contamination sources. Each of the following risk classes is associated with specific aseptic processing manufacturing operations currently in use:
- High-risk: Practiced by 503A and 503B compounding pharmacies, small start-up biologic and drug manufacturers, clinical drug manufacturers, radiopharmaceutical, biologics, and ATMP (Advanced Therapy Medicinal Products)
- Medium-risk: Predominantly practiced by many generic drug manufacturers, contract manufacturing organizations (CMOs) and some smaller new drug or biologic manufacturing companies
- Low-risk: Predominantly practiced by major drug and biologics manufacturing companies and slowly being adopted by generic drug manufacturers, CMOs, and other drug manufacturers
Drug and biologics manufacturers should carefully evaluate the risk class that applies to their aseptic manufacturing process. The practice of high-risk aseptic processing should be avoided unless a firm can repeatably demonstrate that it has a highly trained workforce and appropriate controls to mitigate contamination risks. Even in facilities that utilize sterile-to-sterile drug transfers, there is an approximately 37% chance of contamination of the drug product, for example, due to needle penetration through a vial rubber septum when microorganisms have not been effectively removed from the septum.
Environmental monitoring evaluates processing and operational task suitability and the cleanliness levels achieved in cleanroom and work environments used during aseptic processing. Moreover, an effective environmental monitoring system is a prerequisite that must be established before aseptic operations commence. (Additional information on environmental monitoring can be found in PDA’s Technical Reports No. 13 (Revised 2022) and 13-2 (2020).
All aseptic drug manufacturers should consider using low-risk aseptic processing to ensure that patients, who are often in poor health, receive the highest level of protection against infection when they receive ophthalmic or injectable drug products. The diligent application of low-risk aseptic processing could reduce patient adverse events, recalls and drug shortages. Although low-risk aseptic processing may have higher initial costs due to design, low-risk aseptic processing could reduce the cost of manufacturing due to lower facility, labor and cleaning costs.
The following analysis identifies significant issues in high-risk-class aseptic processing and provides the best practices that should be utilized. A firm must understand and follow all regulatory guidance as a prerequisite to its aseptic filling operations. This article does not address terminally sterilized drug products. Subsequent articles will address medium and low-risk aseptic processing.
High-Risk Aseptic Processing (Manual Filling, Open Containers)
Tasks associated with this risk category include:
- Manual facility cleaning and disinfection
- Cleaning of components
- Preparation of bulk solutions
- Sterilization of components and equipment
- Aseptic filling of primary containers
- Aseptic sealing of primary containers
In high-risk operations, the distance of personnel from open containers or access ports is critical in determining contamination risk. The closer a person or any part of their body is to open containers or access ports/ IV spike needles, the higher the risk of contamination.
Proper Design of the Cleanroom and ISO 5 Equipment
Cleanrooms should be constructed with enough space to allow all work tasks to be conducted without interference from other workspaces. The proper flow of materials, supplies and finished drug products should be designed to follow a one-flow from entry to exit from the workspace. This linear flow can minimize the chance of contamination. There should be adequate storage space designed to accommodate anticipated production volumes, and provisions should be made to ensure that materials do not block return air vents. Furthermore, doors should have automatic, touchless controls with airlocks rather than door handles, and air/material locks should be used when moving from a less-clean area to an area of higher cleanliness with controls that prevent both doors from being open at the same time except for emergency egress.

All surfaces used for the cleanrooms and floors should be compatible with the cleaning agents and the drugs that will be produced. Heating, ventilation and air conditioning (HVAC) systems should be designed by experienced pharmaceutical cleanroom fabricators or contractors that follow pharmaceutical engineering standards. Temperature, humidity and air pressure controls are critical to minimizing microbial contamination from outside environments. Lower temperatures should be maintained to provide comfort to personnel and avoid sweating that would defeat protective clothing barriers.
Prior to purchasing equipment that meets ISO 5 grade air, which is a space that has been classified to meet ISO 14644-1 requirements (3,520 particles/cubic meter) for airborne 0.5 μm particulate in the in-operation state, an ergonomic design analysis that addresses microbial and particulate contamination risks and safe personnel movements should be completed. The analysis will specify the proper size, features and construction of biological safety cabinets (BSCs) or unidirectional flow. Properly designed BSCs or horizontal laminar airflow hoods are recommended to reduce potential contamination from personnel. The actual aseptic work zone within the equipment should be established using dynamic smoke studies, showing areas of minimal turbulence and unidirectional airflow. Vertical airflow-design laminar airflow hoods are not recommended but may be acceptable if effective employee training, oversight and ergonomic process designs are implemented.
Routine calibration and certification of high-efficiency particulate air (HEPA) filters and control equipment are essential to proper facility operation and can provide early warning of a contamination control failure. HEPA filters, control dampers, control systems, humidifiers, heat exchangers and pressure fans/fan drive belts can all fail over time. They should be included in a preventive maintenance program that utilizes the mean time between failure calculations, allowing allow a company to schedule maintenance before equipment fails and thereby preventing contamination events.
Personnel Flow
Personnel flow should be designed to allow one entry into a gowning room and, after gowning, entry into the cleanrooms. A separate exit pathway should be in place to prevent cross-contamination. Space limitations may prevent a separate entry and exit, but this should only be allowed when strict personnel movement procedures prevent personnel from entering and leaving the cleanrooms simultaneously. Personnel movement within the cleanrooms should be designed to prevent employees from becoming a source of cross-contamination.
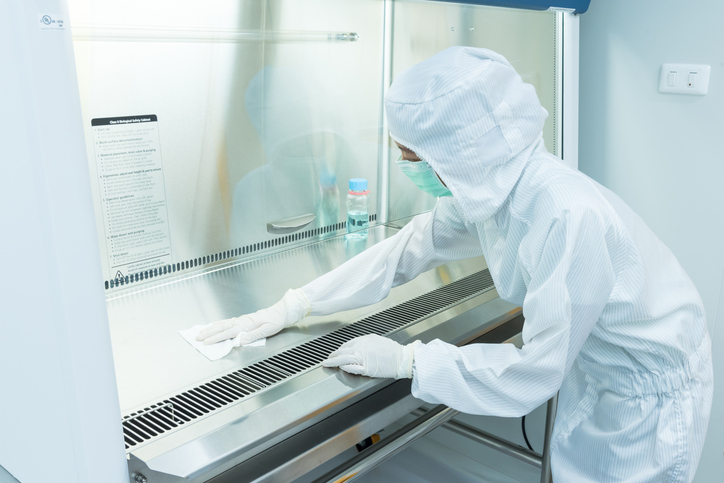
Personnel Gowning and Aseptic Practices
The foundation of personnel gowning and aseptic practices relies on employees being taught effective personal hygiene practices. Personal hygiene practices should not be assumed to be practiced by all employees. Training and verifying all employees in aseptic operations to establish a baseline for acceptable personal hygiene practices is a best practice. This is the first line of defense to minimize microbial contamination.

Personnel wearing street shoes or personal clothing except underwear in work areas is not recommended. Personal clothing and street shoes can have elevated levels of particulates (dust, hair, pollen, pet dander and dirt) on them that could be transferred into cleanrooms if worn under sterile garments. Even if an employee wears freshly washed clothing, the act of going to work can expose the employee and their clothing to numerous contamination sources. There should be a locker room where personnel remove street clothing and shoes and then wash their hands with soap. Additionally, there should be dedicated plant uniforms with long-sleeve shirts that are made of low particle-shedding cloth and dedicated plant shoes.
Protection of the drug product from employee-associated microbial contamination is a fundamental requirement for aseptic processing. Wearing sterile protective garments such as face masks, coveralls, hoods, gloves and goggles is mandatory to minimize the transfer of microorganisms from people to the environment and drug products. The sterile garments used should be selected for ease of donning and an appropriate standard operating procedure (SOP) should be followed that will prevent nonsterile clothing, skin, or hair from contacting the outer surfaces of the garment. Garment suppliers should be able to provide proof of sterility for each batch of garments received and should provide them folded and prepared for ease of donning. Not all sterile garments on the market have the same ability to contain personnel-generated particles and microorganisms, however. The garment supplier should be able to demonstrate the retention levels of particles and microorganisms for the garments chosen (3). Personal comfort and reduction of bellow effects should also be determined for the garments to be included in the gowning procedure.
All outside surfaces of garment packages are contaminated, and proper cleaning and disinfection of the surfaces should occur before opening. The packages themselves should be designed to minimize particulate generation during opening. Sterile gloves should be donned without touching the outside of the glove and disinfected after every touch of a surface or on a routine basis while they are worn. Sterile 70% isopropyl alcohol is a recommended disinfectant and surfactant for gloves if properly saturated.
Sterile tools such as forceps, tweezers, holders or manipulators should be used to contact surfaces of vials, stoppers, seals, syringes, plungers and IV bag ports. The longer the tool, the less chance of contamination by personnel. Stoppers, plungers and plugs should not be placed on work surfaces during processing. Tubing and needle holders should be at least eight inches in length when measured from hand to tip of holder. All personnel should have extensive training in aseptic practice before completing aseptic process simulation (media fill) qualification. PDA offers excellent courses that teach proper aseptic technique, donning of sterile garments and appropriate behavior in the cleanroom (4). Additionally, the FDA’s Center for Compounding Excellence offers online courses that address gowning and aseptic practices.
Media-fill qualifications for personnel should duplicate actual manufacturing operations, including filling duration and type of products filled. A second-person observation or video recording of media-fill qualifications should be performed to document practices of concern or deviations from SOPs.
Ready-to-Sterilize or Ready-to-Use Components
Firms must ensure that suppliers of ready-to-sterilize or ready-to-use components have designed effective cleaning processes and are using cleanroom-appropriate protective packaging; low particulate shedding provides contamination protection for components. Suppliers should use laminar airflow hoods (horizontal or vertical airflow designs) and/or separate cleanrooms for manual cleaning and preparing components. Supplier employee behavior, oversight and the use of ergonomic process designs are essential to reduce the risk of microbial contamination. Firms should use their suppliers’ audit programs or quality agreements to determine whether the quality requirements needed for their components are met.
Design of Material Flow and Usage
Firms must design effective processes to transfer materials from warehouses to support areas to process cleanrooms and into BSCs, reducing access barrier systems or isolators. Soil and microbial contamination can occur while components and supplies are in transit from the original manufacturer’s facilities until materials are processed into the cleanrooms for use in drug manufacturing. These contaminants need to be removed from outside surfaces of packages when packages are transferred from a dirtier area to a cleaner area since mostly manual processes are employed and contaminants can be easily transferred during each stage of entry from warehouse to ultimate use in an ISO 5 class filling zone.
Design of Component and Equipment Cleaning, Sterilization and Usage
Design, purchase and implementation of proper cleaning equipment are critical to removing soil and debris from components before use. Equipment must be designed to gently handle the components to avoid particle generation. Also, cleaning processes should be designed to remove soil, microorganisms, endotoxins, exotoxins, hydrocarbons, lubricants and mold release agents. Qualification of the cleaning processes should be designed to assess the removal of each type of contaminant. Purchase of purified water, water for injection, compressed air or nitrogen (gas or liquid) needs to be sourced from reputable suppliers and have certificates of analysis for each batch received. These materials must be effectively controlled upon receipt, storage and use to prevent contamination of components during cleaning and sterilization/depyrogenation. Containers of these materials can be significant sources of contamination once opened. Compressed gases used during processing need to be sterile-filtered and, if gases are compressed on site, the compressors should be oil-free and have systems to remove water from the compressed gas storage tanks since storage tanks have been found to be significant sources of microbial contamination (5).
Another significant problem that must be addressed is storage time after cleaning, which could allow microorganisms to proliferate on wet components waiting to be sterilized or depyrogenated. Hold-time studies during storage must be conducted to determine the maximum time components can remain wet before further processing. With effective planning, components should be processed as soon as possible after cleaning. Additional information can be found in PDA’s Technical Report No. 69: Bioburden and Biofilm Management in Pharmaceutical Manufacturing Operations.
Cleanroom-designed transfer bags/containers should be utilized to store components after cleaning and sterilization. Firms must ensure that the bags/containers used are clean and particle-free prior to use. Reusable containers must have qualified cleaning processes established before use and suitable storage methods that prevent recontamination before use.
All components being processed should be properly identified for the stage of processing, and segregation methods should be established to prevent mix-ups that could allow components that are not cleaned to be used.
Cleaning and Disinfectant Issues
Personnel and processing operations all contribute contaminants to cleanroom air and surfaces, which environmental contamination studies have repeatedly demonstrated (6-7). Cumulative effects over time can allow microorganisms to be present in the cleanroom air and on work surfaces, including equipment and stainless-steel benchtops. Environmental contamination has been observed even where full sterile gowning is used. Effective cleaning procedures must be designed to remove all previous drug products, particulate matter and microbial contaminants from equipment contact surfaces and cleanrooms. Cleaning agents, disinfectants and sporicides should have low chemical residues, or there should be procedures in place designed to remove residues on a periodic basis.
Another source of contamination routinely found in high-risk aseptic processing is dirty cleaning equipment, utensils, buckets and mops. This equipment should be cleaned and sterilized after each use, stored in proper locations and protected from contamination during storage. Surface disinfectant or sporicide wet-contact times are routinely ignored by personnel assigned to cleaning and must be strictly enforced to ensure that surfaces are thoroughly cleaned. Many facilities rely on ready-to-use, presterilized cleaners, disinfectants and sporicides, but some firms are still observed to be using nonsterile materials. Facilities must ensure that sterilization of cleaning, disinfecting and sporicidal agents has occurred and that cleaning wipes, mop heads and utensils are also sterilized before use or are purchased sterile.
The complexity of high-risk aseptic processing is often overlooked by the firms using this methodology. Operational designs should be objectively scrutinized to ensure that contamination risks are minimized, and human factor analysis has been used to reduce operational errors that could jeopardize the sterility of the drug products being produced. Additional information can be found in PDA’s Technical Report No. 62: Recommended Practices for Manual Aseptic Processes.
Summary
Understanding the microbial contamination risks associated with each type of aseptic processing currently used to manufacture drug products is important. This article provides information for aseptic compounders and manufacturers to consider when they design their aseptic process; the information can also be used to improve their aseptic filling operations and reduce contamination risks. The best practices needed for this high aseptic risk class should be incorporated into each firm’s aseptic filling operations. Knowledge of the sources and types of contamination can be used to train personnel involved in aseptic process design, facility construction, equipment design, preparation of SOPs and operations. Moreover, effective and persistent training in how to reduce or eliminate microbial contamination is essential to manufacturing aseptic drug products.
Due to the significant contamination risks associated with high-risk aseptic filling, it is strongly recommended that manual aseptic filling not be used to prepare sterile drug products in facilities that are poorly designed or where personnel do not have the knowledge or experience to properly conduct aseptic operations. Even if facilities are properly designed and operated by disciplined and knowledgeable personnel, the risk of fatigue and complacency may only allow small quantities of biologics and drug products to be prepared and administered when the treatment benefits clearly outweigh the risks. Nonetheless, advances in automation and robotics have clear advantages over high-risk aseptic processing and, when possible, these low-risk aseptic methodologies should be used in place of manual aseptic processing.
Alternatively, meticulously designed terminal sterilization (heat, steam, chemical or radiation) processes should be evaluated to determine if a drug product will not be degraded by terminal sterilization. This is often an overlooked low-risk aseptic process.
Patients who receive aseptically filled drug products assume that the drugs are sterile and their health will not be negatively affected by microorganisms that could cause hard-to-treat infections and potentially lead to death. Aseptic drug manufacturers must ensure that this scenario does not happen.
The following resources should be used as a company evaluates their aseptic processes:
- PDA Technical Report No. 54: Implementation of Quality risk Management for Pharmaceutical and Biotechnology Manufacturing Operations
- PDA Technical Report No. 69: Bioburden and Biofilm Management in Pharmaceutical Manufacturing Operations
- PDA Technical Report No. 90: Contamination Control Strategy Development in Pharmaceutical Manufacturing
- PDA Technical Report No. 34: Design and Validation of Isolator Systems for the Manufacturing and Testing of Healthcare Products
- PDA Points to Consider of the Aseptic Processing of Sterile Pharmaceutical Products in Isolators
Part three of this article will discuss medium-risk and low-risk aseptic processing.
The following table summarizes the potential for contamination by sources and common types of contaminants for high-risk aseptic processing.| Contamination Sources | Explanation |
|---|---|
| Personnel | People working in the cleanrooms and close to open containers can induce turbulence and eddies in the air near open containers, which can allow contaminants to enter the units being filled. Poor personnel discipline and supervision cause deviations from aseptic practices and result in drug product contamination. Untrained personnel or contractors can cause significant contamination events to occur.
Poor training programs for all levels of personnel and contractors contribute to the lack of personnel understanding and use of improper aseptic techniques or contract services. |
| Components and Supplies | Manual use of disinfectants to clean surfaces of containers during transfer from one clean zone to another for ready-to-use components may not be performed correctly and risk microbial contaminants remaining on package surfaces and entering the aseptic filling zones.
Even sterile-to-sterile compounding increases the risk of contamination due to external contaminants on vials and syringes during storage and use. APIs and components could have endotoxin and exotoxin contaminants present in quantities that could cause physiological harm. |
| Liquids | Manual manipulation of filters and use of improper grade filters are common problems. Some solutions are filtered into the ISO 5 filling area but are stored for periods of time that could allow contamination ingress if not properly sealed and stored. |
| Tools | Tool cleaning and disinfection are manual processes where human variability can prevent removal of microorganisms. |
| Equipment | Tubing and pumps can cause contamination if not carefully selected for aseptic processing. Hand tools used may place the hand close to open containers. Hand-crimping tools or plunger-placement tools can be significant sources of contamination.
HEPA-filter or filter-seal failures on laminar flow units or BSCs and leaks in negative pressure isolators, if not detected and fixed, will allow airborne microorganisms to contaminate the drug products being filled. |
| Processes | Lack of ergonomic design increases the risk of contamination. The use of first air principles is critical to reduce contamination risk. |
| Facilities | Poor construction practices and materials of construction can cause significant episodes of microbial and particulate contamination.
Cleanrooms in these facilities may not provide adequate segregation of classified rooms from nonclassified areas surrounding the ISO 5 workspaces. The use of handwashing sinks in anterooms can be a source of microbial contamination during gowning. Gaps in ceiling tiles, cracks in walls and floors with cracks can lead to persistent levels of microbial contamination. Door handles can allow microorganisms to be transferred between personnel. Poorly monitored air pressure differentials and open doors can cause the mingling of air containing microbial spores to enter the cleanrooms. Water leaks or poorly maintained HVAC cooling coils are significant sources of mold and fungi contamination. Cleanroom HEPA-filter or filter-seal failures, if not detected and fixed, will allow airborne microorganisms to contaminate the drug products being filled. Negative-pressure cleanrooms that are not properly sealed will allow microorganisms and particulate matter to contaminate the room. |
| Skin Cells and Hair | Skin cells and hair present in cleanrooms can contaminate ISO 5 work areas during processing due to venturi effects and personnel intrusion or poor aseptic manipulation practices. |
| Fibers | Clothing, containers and cleaning supplies are the most likely sources of fibers, and there is a high risk that they may be present in ISO 5 work zones during all manual processes. |
| Dust | Cleanrooms rely upon air filtration processes to control dust, but it may be present on personnel or materials in the cleanrooms or ISO 5 filling zones. |
| Bacteria | Bacteria are present in the cleanrooms when personnel are present and when materials are moved. If cleaning/disinfecting procedures are not adequate to maintain a facility, and/or when facility or equipment used are not suitable for aseptic operations, they will continue to be present. |
| Fungi | Fungi are present in the cleanrooms when:
|
| Viruses | Viruses are present in the cleanrooms when personnel are present, organic materials are used and cleaning/disinfecting procedures are not adequate to maintain the equipment. |
| Lubricants | Depending on the source and the use of equipment, lubricants can be a source of contamination, for example, seal failure. |
| Metals | Due to manual processes, unless mixers are used post-filtration, there is a low probability of metals presenting a source of contamination. |
| Component Particles | Component particles are likely to be present in cleanrooms. Firms may rely upon component vendors to reduce particulates and recommend component types. Many of these facilities rely upon ready-to-use or ready-to-sterilize prepackaged components. Contamination sources are dirt accumulated during shipping, packaging material and poorly cleaned components. |
| Chemical Residues (Cleaning Agents and Previous Drug Products) | A manual cleaning process can allow chemical residues to accumulate over time. |
References
- Microbial Control of Raw Materials Used in Pharmaceuticals. www.pda.org. https://www.pda.org/pda-letter-portal/home/full-article/microbial-control-of-raw-materials-used-in-pharmaceuticals.
- Office of Regulatory Affairs. Recalls, Market Withdrawals, & Safety Alerts. U.S. Food and Drug Administration. https://www.fda.gov/safety/recalls-market-withdrawals-safety-alerts.
- Eaton t., Whyte W., 2021, Effective Reusable Cleanroom Garments and Evaluation of Garment Life, EJPPS European Journal of Parenteral and Pharmaceutical Sciences, January 2021 DOI: 10.37521/ejpps.25401.
- PDA Training | Continuing Education for Pharmaceutical Manufacturers. www.pda.org. https://www.pda.org/pda-training/home.
- Bajerski F, Nagel M, Overmann J. Microbial occurrence in liquid nitrogen storage tanks: a challenge for cryobanking? Appl Microbial Biotechnology. 2021 Oct;105(20):7635-7650. doi: 10.1007/s00253-021-11531-4. Epub 2021 Sep 24. PMID: 34559283; PMCID: PMC8460408.
- Favero et. al., 1966, Comparative Levels and Types of Microbial Contamination Detected in Industrial Clean Rooms, Applied Microbiology, July, Vol. 14, No.4.
- Sandle, T. (2011): ‘A Review of Cleanroom Microflora: Types, Trends, and Patterns’, PDA Journal of Pharmaceutical Science and Technology, Vol. 65, No.4, July–August 2011, pp392-403


 David Jaworski is PDA’s Sr. Advisor for Scientific Affairs. He was a Senior Policy Advisor at U.S. Food and Drug Administration for more than seven years and had previously worked in the CDER Office of Compliance as a Consumer Safety Officer and as Acting Branch Chief in the Domestic Case Branch. His experience in the pharmaceutical industry encompasses over 22 years in business management, research, manufacturing and consulting.
David Jaworski is PDA’s Sr. Advisor for Scientific Affairs. He was a Senior Policy Advisor at U.S. Food and Drug Administration for more than seven years and had previously worked in the CDER Office of Compliance as a Consumer Safety Officer and as Acting Branch Chief in the Domestic Case Branch. His experience in the pharmaceutical industry encompasses over 22 years in business management, research, manufacturing and consulting.